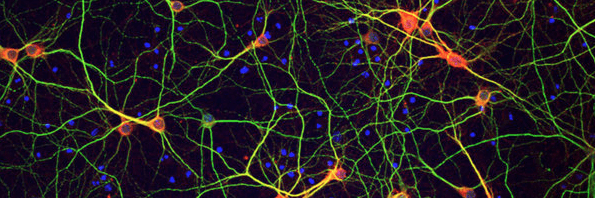
 A holistic, integrative approach can often slow the neurodegenerative processes that underlie Alzheimer’s disease, Parkinson’s, and many other neurological conditions.
A holistic, integrative approach can often slow the neurodegenerative processes that underlie Alzheimer’s disease, Parkinson’s, and many other neurological conditions.
Carefully tailored nutritional and lifestyle changes can also strengthen the central and peripheral nervous systems, decrease oxidative stress, and optimize mitochondrial function.
But neurodegenerative disorders are typically very complicated, with multiple comorbidities, so it can be difficult even to know where to begin when working with patients and their families.
In my experience, toxin elimination is a very good starting point.
The link between Parkinson’s disease (PD) and toxicant exposures is well established. The link between heavy metals and multiple sclerosis (MS) is also highly suggestive. Environmental exposures have also been implicated in amyotrophic lateral sclerosis (ALS).
This certainly doesn’t mean everyone that has been exposed to high numbers of toxins will develop neurodegenerative diseases. Genetic vulnerability is always at play, and the very apt saying applies here: “Genetics loads the gun and environment pulls the trigger.”
But toxins do play a role, and it is worth assessing for toxic exposures in patients showing signs and symptoms of neurodegenerative diseases.
The Toxin ConnectionAssessment for “acute” heavy metal exposure, and urine tests for more “chronic” heavy metal toxicity make a lot of sense in this context.
The technical definition of “acute” really means exposure to large amounts of heavy metals at one time, or on a routine daily basis as in some occupational situations. In the United States, the Agency for Toxic Substances and Disease Registry helps to further define acute exposures.
Though there are clear clinical guidelines for treating acute heavy metal poisoning, unfortunately no such guidelines exist for chronic low-level exposures. This makes heavy metal testing difficult to interpret. How do we know when to undertake detoxification treatments?
We can find some guidance, by comparing a patient’s test results to the numbers posted in the CDC’s National Report on Human Exposure to Environmental Chemicals. This data is updated one to two times per year.
For a patient whose test data indicate that he or she is in the 80th percentile or above for a given toxin, I treat. I do this mostly through sweat depuration, exercise to tolerance, and high fiber diets to reduce enterohepatic redistribution of toxins.
I also recommend supplementing with:
- Glutathione and alpha lipoic acid;
- N-acetylcysteine
- Vitamin C
- Probiotics (Ibrahim F, et al. Can J Microbiol. 2006;52(9):877-85. ).
Occasionally, if the body burden of a given toxin is very high, I’ll recommend oral heavy metal chelators.
Assess Inflammatory Markers
I find it is also useful to look at the status of key vitamins, minerals, hormones, as well as markers of inflammation.
These include: Iron; Thyroid stimulating hormone [TSH], free thyroxine [FT4], and free triiodothyronine [FT3]); Methylmalonic acid levels and B12; Vitamin E; Homocysteine (; Dehydroepiandrosterone sulfate (DHEA-S); Pregnenolone; Testosterone; Estrogen; Vitamin D (25(OH)D3); Lipids; and Inflammatory markers.
 Consider Infections
Consider Infections
Another area to consider is that of infectious triggers and overall pathogen load. Depending on the case history and physical exam, I may think about tick-borne illnesses and viral insults as underlying factors driving the neurological symptoms. The index of suspicion for an infectious trigger goes way up if the patient is experiencing extreme fatigue.
Quantitative titers of Epstein Barr Virus (EBV), Cytomegalovirus (CMV) and herpes simplex 6 (HSV-6) may help elucidate the etiology of some signs and symptoms.
Think about testing for Helicobacter pylori if the signs and symptoms are suggestive. Eradication of H. pylori can sometimes lead to improvements in dementia and other neurodegenerative conditions.
Stool cultures for assessment of the gastrointestinal microbiome may also be very helpful (Smith PA. Nature. 2015; 15;526(7573):312-4). All of these tests can provide a picture of a patient’s infectious load, which can activate the immune system and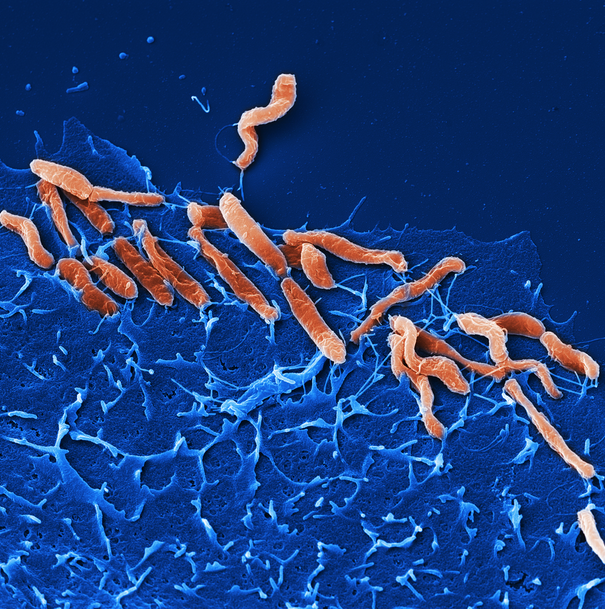 contribute to chronic inflammation—a key driver of neurodegeneration.
contribute to chronic inflammation—a key driver of neurodegeneration.
Mediterranean Adaptations
I recommend that all my patients with neurodegenerative diseases go on a gluten-free, anti-inflammatory diet, which includes lots of low glycemic organic fruits and vegetables, such as blueberries, apples, pears, Brussels sprouts and asparagus.
This approach is essentially an adaptation of the traditional Mediterranean diet, minus gluten and—in most cases—the dairy. I recommend this diet because studies show that the Mediterranean diet is inherently anti-inflammatory. It can also improve white matter lesions (Gardener H, et al. Arch Neurol. 2012; 69(2):251-6) and mitigates neurodegeneration (Sofi F, et al. Curr Nutr Rep. 2013: 2 (2): 75–80).
I also suggest drinking as much organic green tea as possible, as polyphenols have been shown to be helpful in neurodegenerative diseases. Decaffeinated green tea is fine. In fact, in some individuals, caffeine may worsen symptoms.
Nutrαceutical Interventions
There are a host of supplements and nutraceuticals that can be helpful in mitigating the symptoms and slowing the progression of neurodegenerative diseases. Note that the large dose ranges listed below reflect the need to individualize and tailor the regimens to each patient’s unique health and nutritional status, and symptom profile.
Some patients may not be able to tolerate the higher doses indicated. The studies cited typically use single nutrients aimed toward specific pathological targets, rather than complex combination formulas. Theoretically, one could use lower doses, if one is using multiple products or formulas to simultaneously target multiple pathogenic mechanisms.
For simplicity, the recommendations below are total daily oral doses (not intramuscular or intravenous doses):
- N-Acetyl Cysteine: 600-1,200 mg (Bavarsad S, et al. Brain Behav. 2014)
- Acetyl-Glutathione: 400-1,000 mg (Bains JS, et al. Brain Res Brain Res Rev. 1997)
- Alpha Lipoic Acid (ALA): 300-1,200 mg (Moreira PI, et al. Biochim Biophys Acta. 2010)
- Coenzyme Q10: 400-800 mg. Note that you can use lower amounts if using ubiquinol (Mancuso M, et al. Curr Drug Targets. 2010)
- Acetyl-L-Carnitine: 500-3,000 mg (Calvani M, et al. Ann N Y Acad Sci. 1992)
- Biotin: 300 mg (Sedel F, et al. Mult Scler Relat Disord. 2015)
- Citicoline: 500-3,000 mg (Qureshi I. et al. NMJ. 2010)
- Vitamin B12, as methyl, adenosyl and hydroxocobalamin: 1,000-5,000 mcg (Gröber U, et al. Nutrients. 2013. Izumi Y, et al. Brain Nerve. 2007)
- Lipid Replacement Therapy: 3,000-6,000 mg (Nicolson GL et al. Biochim Biophys Acta. 2014)
- Omega 3 & 6 essential fatty acids: 2,000-6,000 mg EPA/DHA, and 600-1,000 mg Gamma Linolenic Acid (Mehta LR, et al. Nat Clin Pract Neurol. 2009)
- Whole Coffee Berry Extract: 200 mg (Reyes-Izquierdo T, et al. Br J Nutr. 2013)
- Dehydroepiandrosterone (DHEA): 10-50 mg (Goncharov NP, et al. Fiziol Cheloveka. 2013)
- 7-Keto DHEA for females: 100-200 mg
- Pregnenolone: 100-150 mg (Lapchak PA, et al. Int Rev Neurobiol. 2001)
- Vitamin D3: 1,000-5,000 IU (Fernandes de Abreu DA, et al. Psychoneuroendocrinology. 2009)
- Low Dose Naltrexone: 1.5-4.5 mg (https://ldnresearchtrust.org/ldn-clinical-trials)
Further, there are a number of botanicals that can be helpful in slowing progression of neurodegenerative disorders. Here’s a short list:
- Curcumin (Curcuma longa): 1,000-5,000 mg, depending on the form (Kim DS, et al. Recent Pat CNS Drug Discov. 2012)
- Mucuna pruriens (aka Velvet Bean): 400-1000 mg, standardized to 15% L-Dopa. Be careful using Mucuna with patients on L-Dopa agonist medications (Houghton PJ et al. Ethnopharmacology-Vol III.)
- Bacopa monnieri: 150-500 mg (Simpson T, et al. Evid Based Complement Alternat Med. 2015)
- Lion’s Mane mushroom (Hericium erinaceus): 500-3,000 mg (Friedman M. J Agric Food Chem. 2015 and Khan MA, et al. J Complement Integr Med. 2013)
 Though these are all “natural” therapies, none of the above suggestions should be initiated without the guidance of a well-trained clinician. I suggest implementing just a few interventions at a time, based upon the specific condition(s) and symptom patterns a particular patient is experiencing.
Though these are all “natural” therapies, none of the above suggestions should be initiated without the guidance of a well-trained clinician. I suggest implementing just a few interventions at a time, based upon the specific condition(s) and symptom patterns a particular patient is experiencing.
If one attempts to initiate too many simultaneous interventions and there is an adverse reaction, there are too many variables to determine the cause. Further, most patients will find an onslaught of treatments overhelming and expensive and will more than likely not adhere to the recommended regimen.
There are also many combination products on the market, where synergy may play a role and the above dosages can be altered. This has the advantage of lowering overall cost and pill burden.
The suggestions above are by no means a complete list of all the natural therapies that have potential to mitigate neurodegeneration. They’re intended as more of a spark to get you to think about how to help patients with these truly devastating conditions.
END
Todd Born, ND, is a naturopathic physician, certified nutrition specialist (CNS), co-owner and medical director of Born Naturopathic Associates, Inc., in Alameda, CA. Dr. Born graduated from Bastyr University in Seattle, WA and completed his residency at the Bastyr Center for Natural Health and its thirteen teaching clinics, with rotations at Seattle-area hospitals. His clinical focus is on utilizing integrative medicine to mitigate chronic disease. He has a strong interest in difficult and refractory cases, allergies, gastrointestinal issues, neurological and neurodegenerative disorders, endocrinology, cardiovascular disease and diabetes, autoimmune disease, development and behavioral issues, HIV/AIDS, and geriatrics. He is the Product Manager, Head of New Product Development, and Scientific Advisor for Allergy Research Group, and is Editor-in-Chief of the company’s Focus Newsletter.